Significance
Accurate prostate cancer diagnosis is critical in determining the most effective treatment plan for patients. Imaging plays a vital role in the process because it helps in determining the presence, location, and extent of the cancer. Conventional imaging modalities such as transrectal ultrasound (TRUS) commonly used for guiding needle biopsies as well as multiparametric MRI (mpMRI) can provide detailed images that helps in the detection and localization of prostate cancer. While these methods are invaluable, there is a constant search for more specific and sensitive imaging techniques, particularly for detecting cancer recurrence and metastasis. Prostate-specific membrane antigen (PSMA) is a protein expressed abundantly on the surface of prostate cancer cells, making it an excellent target for diagnostic imaging and therapeutic purposes. PSMA-labeled imaging agents have been developed for use in PET/CT and SPECT/CT imaging to detect prostate cancer cells based on their expression of PSMA. While gallium 68 (Ga-PSMA) labeled PSMA PET/CT scans have been extensively researched, the global accessibility and cost-effectiveness of Technetium-99 -PSMA (Tc-PSMA) single-photon emission computed tomography/computed tomography (SPECT/CT) present an attractive alternative, but has not been extensively studied. To this end, a new clinical study published in Prostate Journal and led by Dr. Iain Duncan, Nicholas Ingold from Garran Medical Imaging in Australia alongside Dr. Elisa Martinez-Marroquin and Dr. Catherine Paterson from University of Canberra, the researchers conducted comprehensive study to evaluate the diagnostic accuracy of Tc-PSMA SPECT/CT compared to mpMRI for the diagnosis, staging, and detection of relapse in prostate cancer.
The team recruited 425 men referred for primary staging of prostate cancer and 172 men with biochemical relapse (BCR) after initial treatment. Comprehensive clinical data, including biopsy results, PSA levels, and previous imaging findings, were collected and analyzed. The authors performed Tc-PSMA SPECT/CT imaging on the participants using a novel reconstruction algorithm developed by the researchers. This new technique aimed to improve the diagnostic accuracy of Tc-PSMA imaging by enhancing image quality and resolution. Participants also underwent mpMRI, to compare between Tc-PSMA SPECT/CT and mpMRI in terms of diagnostic accuracy for prostate cancer. Moreover, the authors evaluated the diagnostic accuracy of Tc-PSMA SPECT/CT and mpMRI and evaluated their findings using biopsy as the gold-standard. They also calculated sensitivity, specificity, accuracy, and precision of both imaging modalities. Furthermore, the researchers analyzed correlations between Tc-PSMA uptake and various clinical parameters, including biopsy grade, PSA levels, and the presence of metastases, to evaluate the diagnostic value of Tc-PSMA SPECT/CT.
The authors found that Tc-PSMA SPECT/CT exhibited high diagnostic accuracy in the primary staging of prostate cancer, with sensitivity, specificity, accuracy, and precision surpassing those of mpMRI. This suggests that Tc-PSMA SPECT/CT is highly effective in detecting primary prostate cancer lesions. They also found that in patients with biochemical relapse, Tc-PSMA SPECT/CT demonstrated varying positivity rates at different PSA levels, which indicates its sensitivity in detecting recurrent disease. The study found that the positivity rate increased with higher PSA levels, highlighting the advantage of using of Tc-PSMA SPECT/CT in the surveillance and management of patients’ post-treatment. Moreover, they observed moderate correlations between Tc-PSMA uptake and biopsy grade, PSA levels, and the presence of metastases which suggested that Tc-PSMA SPECT/CT imaging can aid in the diagnosis of prostate cancer and also provide valuable information regarding the aggressiveness and spread of the disease. Furthermore, the study highlighted several advantages of Tc-PSMA SPECT/CT, including its potential for greater accessibility and lower cost compared to Ga-PSMA PET/CT. Additionally, the novel SPECT/CT reconstruction algorithm used in Tc-PSMA imaging offered enhanced sensitivity for primary lesion detection and the capability for intraoperative localization of lymph nodes.
Overall, the significance the research conducted by Dr. Iain Duncan and colleagues is manifold and has promising implications for the future of prostate cancer diagnosis. First, the researchers provided compelling evidence that Tc-PSMA SPECT/CT, particularly with the novel reconstruction algorithm optimized for Tc-PSMA, which offered superior diagnostic accuracy and sensitivity compared to mpMRI in the primary diagnosis and staging of prostate cancer. This enhanced sensitivity is critical for detecting early-stage cancers and accurately staging the disease, which is essential for determining the most appropriate treatment strategies. Secondly, for patients experiencing biochemical relapse, the authors successfully demonstrated the use of Tc-PSMA SPECT/CT in detecting recurrent disease at various PSA levels. This ability to sensitively detect recurrence even at low PSA levels enables timely intervention and adjustment of treatment plans to address the relapse, potentially improving patient outcomes.
In a statement to Medicine Innovates, Dr Duncan summed up the study and said “PET-CT PSMA has dominated this space in the workup of prostate cancer in advanced economies but we have shown that where SPECT/CT is more accessible, it can provide a similar role in the diagnosis and staging of prostate cancer.”
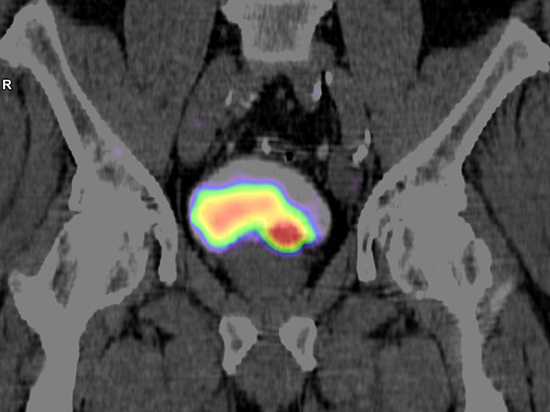
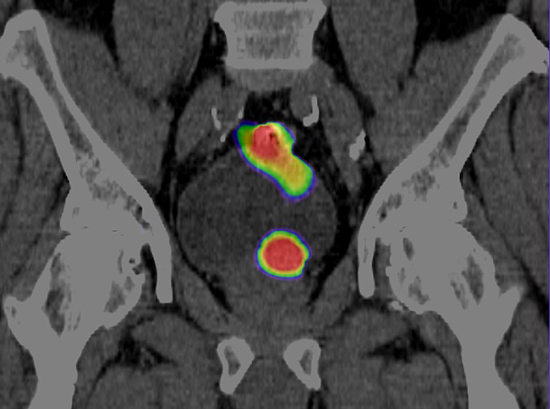
The images are from a Tc-PSMA scan in a 65yr old male with a negative prostate biopsy and PSA=28 (elevated++). MRI was also negative, so a Tc-PSMA was undertaken. The first image (4hr Tc-SPMA SPECT/CT) suggests a possible prostate malignancy at the base of prostate but the proximity of the tracer in the adjacent bladder casts some uncertainty. The second image is taken 24hrs later and confirms the diagnosis (no residual bladder tracer and increasing uptake in the tumour). The tracer seen behind the bladder is physiological tracer in the rectum.
This case demonstrates the high Tc-PSMA tracer uptake in primary prostate lesions often seen with PSMA radioligands. An additional advantage of Tc-PSMA over other ligands and compared with PET tracers is the longer half-life, which allows delayed (24hr) imaging. As see in this case 24hr images have a high target to background ratio and progressive uptake by tumour cells helps differentiate tumour uptake versus benign uptake both in the prostate and elsewhere. The standard biopsy was likely negative because of the difficult to access location. After the Tc-PSMA scan a targeted biopsy confirmed the diagnosis of a high-grade prostate carcinoma.
Reference
Duncan I, Ingold N, Martinez-Marroquin E, Paterson C. An Australian experience using Tc-PSMA SPECT/CT in the primary diagnosis of prostate cancer and for staging at biochemical recurrence after local therapy. Prostate. 2023;83(10):970-979. doi: 10.1002/pros.24538.
 Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity
Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity

