Significance
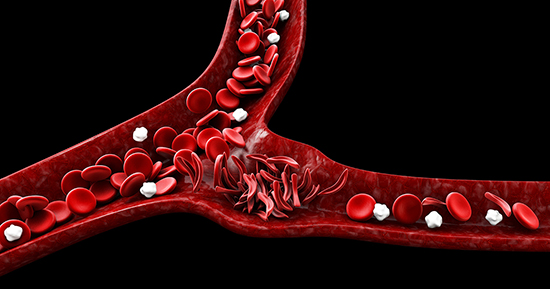
Sickle cell disease (SCD) is a group of inherited red blood cell disorders. It’s characterized by the production of an abnormal form of hemoglobin, called hemoglobin S (HbS). This abnormal hemoglobin causes red blood cells to become rigid, sticky, and misshapen, resembling a crescent or “sickle” shape. SCD is caused by a mutation in the HBB gene, which provides instructions for making beta-globin, a component of hemoglobin. This mutation is inherited in an autosomal recessive pattern, meaning that a child must inherit two copies of the mutated gene (one from each parent) to be affected. If only one copy is inherited, the individual is a carrier (commonly referred to as having sickle cell trait) and usually doesn’t show symptoms. SCD is often diagnosed through blood tests, which can detect the presence of HbS. Newborn screening for SCD is standard in many countries, allowing early diagnosis and intervention. There’s no cure for SCD, but treatments can alleviate symptoms and reduce complications. Research in gene therapy and other novel treatments continues to advance, offering hope for more effective treatments or a potential cure in the future. Because SCD is a monogenic disorder it has been a prime candidate for gene therapy. Early clinical trials have shown promise in using gene therapy to induce the production of fetal hemoglobin, thereby ameliorating the symptoms of SCD. However, the recent cases of myeloid malignancies in gene therapy recipients have cast a shadow over this optimism, necessitating a deeper understanding of the genomic consequences of gene therapy in SCD patients. A new study published in Nature Medicine led by Professor Peter Campbell at Wellcome Sanger Institute & Professor David Kent from York University highlights a complex interplay between gene therapy and hematopoietic stem cell (HSC) dynamics, particularly concerning the emergence of myeloid malignancies.
The research team employed whole-genome sequencing to track the clonal evolution of HSCs in six SCD patients undergoing gene therapy. This approach enabled the detailed mapping of somatic mutations and clonal dynamics in both gene-modified and unmodified HSCs, pre- and post- gene therapy. The patient cohort, part of a clinical trial (NCT03282656), received gene therapy via plerixafor-mobilized CD34+ cells transduced with a vector inducing γ-globin expression. The researchers found a variable mutation burden in pre- gene therapy HSCs, with some patients showing elevated levels compared to age-matched controls. This raised the possibility of SCD or its treatment (like hydroxycarbamide) influencing mutation rates. Interestingly, post- gene therapy, there was an increase in potential driver mutations (particularly DNMT3A and EZH2 mutations) in both modified and unmodified cells, indicating a positive selection of mutant clones during gene therapy.
The study did not identify clonal expansions in the post- gene therapy period, a reassuring finding considering the risk of leukemogenesis. However, the increased frequency of driver mutations post- gene therapy is concerning. It suggests that the gene therapy process, including cell manipulation and engraftment, might confer a selective advantage to HSCs with pre-existing mutations, potentially heightening the risk of clonal expansions and myeloid neoplasms. An important consideration is the long-term behavior of these mutant clones. While the study’s timeframe did not allow for conclusive observations, the potential for these clones to contribute to myeloid malignancies cannot be ignored. This necessitates ongoing surveillance and research into the mechanisms driving clonal expansion in the context of gene therapy.
The findings pose significant implications for patient selection and monitoring in gene therapy trials. Screening for pre-existing driver mutations might become crucial, although the sensitivity of current technologies is a limiting factor. Furthermore, this study emphasizes the need for minimizing additional mutations pre- gene therapy, possibly advocating for earlier intervention. This research underscores the necessity for a holistic understanding of gene therapy impacts, particularly in the context of clonal hematopoiesis and mutation dynamics. Future studies should focus on identifying the specific aspects of the gene therapy process that favor clonal selection and expansion, which could lead to more refined and safer gene therapy approaches.
The study by Campbell and Kent marks a significant step in understanding the genomic landscape of SCD in the context of gene therapy. While it offers reassurance in some aspects, it also raises critical questions about the long-term implications of gene therapy, particularly regarding the selection and expansion of mutant HSC clones. These findings are pivotal in guiding future gene therapy trials, emphasizing the importance of comprehensive genomic surveillance and the need for continuous refinement of gene therapy methodologies. As we stride towards a cure for SCD and other genetic disorders, it is imperative that we balance the promise of these advanced therapies with an understanding of their complex biological implications. This research not only contributes to the field of SCD treatment but also serves as a valuable reference point for the broader application of gene therapy in various hematological conditions.
Reference
Michael Spencer Chapman, Alyssa H. Cull, Marioara F. Ciuculescu, Erica B. Esrick, Emily Mitchell, Hyunchul Jung, Laura O’Neill, Kirsty Roberts, Margarete A. Fabre, Nicholas Williams, Jyoti Nangalia, Joanne Quinton, James M. Fox, Danilo Pellin, Julie Makani, Myriam Armant, David A. Williams, Peter J. Campbell, David G. Kent. Clonal selection of hematopoietic stem cells after gene therapy for sickle cell disease. Nature Medicine, 2023; DOI: 10.1038/s41591-023-02636-6
 Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity
Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity


