Significance
Platelets, tiny cell fragments involved in blood clotting and wound healing, have long been associated with cancer. Professor Armand Trousseau’s 1865 observation that thrombosis could serve as an early sign of malignancy sparked interest in the relationship between platelets and cancer. Over the years, pre-clinical models have elucidated the intricate interplay between platelets, circulating tumor cells, the tumor microenvironment, and metastasis.
Activated platelets play a multifaceted role in cancer progression. They shield circulating tumor cells from the immune system, facilitate their adhesion to the endothelium, support their migration through blood vessels, and contribute to the formation of metastatic niches. This connection between platelet activation and malignancy has opened doors for potential therapeutic interventions, particularly in the form of aspirin.
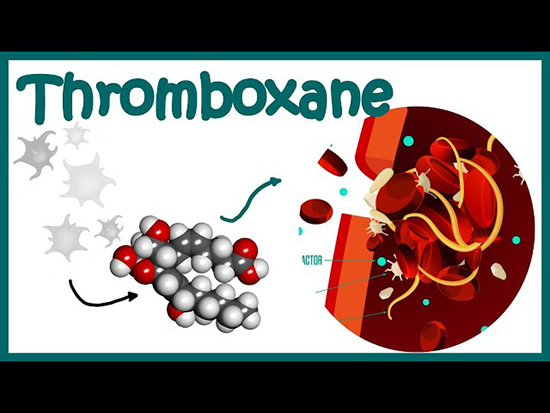
Aspirin, a widely used over-the-counter medication, is known for its anti-inflammatory and antithrombotic properties. At low doses (75-100 mg daily), aspirin irreversibly acetylates cyclo-oxygenase-1 (COX-1) in platelets, primarily inhibiting the production of thromboxane A2 (TXA2). TXA2 is a potent platelet activator that amplifies platelet aggregation and activation in response to various stimuli.
Pre-clinical studies have demonstrated that inhibiting COX-1 in platelets with aspirin can reduce metastasis by impeding the interaction between circulating tumor cells and platelets during intravascular transition. Moreover, research in genetically modified mice has emphasized the connection between COX-1 in platelets and carcinogenesis, particularly in intestinal tumors.
Epidemiological and randomized data have also suggested that daily aspirin use can reduce cancer incidence, particularly in gastrointestinal tumors. For example, aspirin has been recommended for the prevention of colorectal cancer in individuals with Lynch Syndrome based on long-term data from the CAPP2 trial. In a new study led by Professor Ruth Langley at the MRC Clinical Trials Unit-University College London, and published in the British Journal of Cancer, provided new insights into the role of platelet activation in cancer progression and the potential of aspirin as a preventive measure have emerged. This study sheds light on a critical aspect of cancer biology and opens avenues for further research and clinical applications. The study involved 716 patients with various cancer types who had undergone radical cancer therapy. Urinary 11-dehydro-thromboxane B2 (U-TXM), a biomarker of in vivo platelet activation, was measured and correlated with patient demographics, tumor type, recent treatment, and aspirin use. The key findings of the study are as follows:
Elevated U-TXM Levels: Patients with cancer, even after radical therapy, exhibited persistently increased thromboxane biosynthesis, as reflected by higher U-TXM levels compared to healthy individuals.
Variations by Tumor Type: The study revealed significant variations in U-TXM levels among different tumor types, with colorectal and gastro-oesophageal cancer patients exhibiting the highest levels.
Influence of Baseline Characteristics: U-TXM levels were associated with various baseline characteristics, including higher body mass index, inflammatory markers, and platelet counts.
Aspirin’s Impact: Daily aspirin use (100 mg) resulted in a substantial reduction (median reductions of 77-82%) in U-TXM levels across all tumor types. Interestingly, aspirin at a higher dose (300 mg) did not provide additional suppression of U-TXM compared to the 100 mg dose.
Biomarker for Active Malignancy: The study suggests that thromboxane biosynthesis, as indicated by U-TXM levels, could serve as a biomarker for active malignancy. This could potentially aid in identifying patients who are likely to benefit from aspirin therapy.
The variation in U-TXM levels among different tumor types underscores the complexity of cancer biology. Aspirin’s efficacy and its role in preventing metastasis may vary depending on the tumor’s molecular characteristics and microenvironment.
Precision Medicine Approach: Understanding the mechanism underlying aspirin’s anti-cancer effects could pave the way for a more precise and personalized approach to its use in oncology. Tailoring aspirin therapy based on individual patient characteristics and tumor type may optimize its benefits.
The association between platelet counts and thromboxane biosynthesis raises the possibility of using platelet counts as an early indicator or screening tool for cancer risk. Further research in this area could be promising.
Aspirin Dosing: The study’s findings on aspirin dosing provide valuable insights. Low-dose aspirin (100 mg) appears to be as effective as a higher dose (300 mg) in suppressing platelet activation. This information can guide clinical practice and minimize potential side effects.
The study led by Professor Ruth E. Langley sheds light on the critical role of platelet activation in cancer progression and the potential of aspirin as a preventive measure. It underscores the need for further research to unravel the complex interactions between platelets, tumor biology, and aspirin’s mechanisms of action. As we move toward a more personalized approach to cancer prevention and treatment, these findings offer hope for more targeted and effective strategies in the fight against cancer.
Reference
Joharatnam-Hogan N, Hatem D, Cafferty FH, Petrucci G, Cameron DA, Ring A, Kynaston HG, Gilbert DC, Wilson RH, Hubner RA, Swinson DEB, Cleary S, Robbins A, MacKenzie M, Scott-Brown MWG, Sothi S, Dawson LK, Capaldi LM, Churn M, Cunningham D, Khoo V, Armstrong AC, Ainsworth NL, Horan G, Wheatley DA, Mullen R, Lofts FJ, Walther A, Herbertson RA, Eaton JD, O’Callaghan A, Eichholz A, Kagzi MM, Patterson DM, Narahari K, Bradbury J, Stokes Z, Rizvi AJ, Walker GA, Kunene VL, Srihari N, Gentry-Maharaj A, Meade A, Patrono C, Rocca B, Langley RE. Thromboxane biosynthesis in cancer patients and its inhibition by aspirin: a sub-study of the Add-Aspirin trial. Br J Cancer. 2023 Sep;129(4):706-720. doi: 10.1038/s41416-023-02310-1.
 Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity
Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity

