Significance
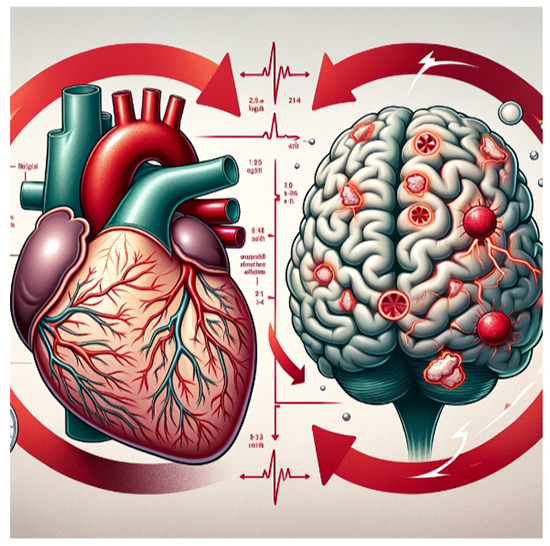
Atrial Fibrillation (AF) is a common type of heart arrhythmia, characterized by an irregular and often rapid heart rate. It occurs when the two upper chambers of the heart (the atria) beat chaotically and out of sync with the two lower chambers (the ventricles). This can lead to a variety of symptoms, including heart palpitations, shortness of breath, weakness, and reduced ability to exercise. There is growing evidence suggesting a link between Atrial Fibrillation and an increased risk of developing dementia. It is believed AF can lead to an inconsistent blood flow to the brain. Regular heart rhythms help to ensure a consistent blood supply, but the erratic heartbeats in AF can disrupt this, potentially leading to reduced blood flow to the brain. Moreover, AF significantly increases the risk of stroke. When the heart doesn’t beat properly, blood can pool and form clots in the atria. If a blood clot forms, it can travel to the brain, leading to a stroke. Strokes can cause brain damage, which is a risk factor for certain types of dementia. Additionally, AF may contribute to cerebral small vessel disease, a condition in which the small arteries in the brain are damaged. This damage can also contribute to the development of dementia. It is also believed that AF can lead to chronic inflammation in the body, which has been linked to the development of dementia. Inflammation can damage brain cells and contribute to the decline in cognitive functions. It is noteworthy to mention that both AF and dementia share common risk factors such as high blood pressure, diabetes, and age. These overlapping risk factors can contribute to the development of both conditions.
In a new study published in the Journal of the American College of Cardiology by Sheng-Chia Chung PhD, Martin Rossor MD, Ana Torralbo PhD, Cai Ytsma MSc, Natalie K. Fitzpatrick MSc, Spiros Denaxas PhD, and led by Professor Rui Providencia MD, PhD from the University College London investigated the association between atrial fibrillation (AF) and the development of mild cognitive impairment (MCI), along with its progression to dementia. The study spanned from January 1, 1998, to May 31, 2016. The researchers included all individuals with incident AF and defined the index date as the date of the first recorded AF diagnosis. For each case of AF, a control individual without AF was randomly selected from the study cohort. These controls were matched to the cases based on sex and age at the diagnosis of AF. AF was identified using ICD-10 codes and corresponding Read version 2 terms from the Clinical Practice Research Datalink.
A key aspect of the study was the use of the UK-based linked electronic health records (EHR), which provided a rich source of data for analysis. The researchers defined AF based on ICD-10 codes and included a comprehensive set of variables such as socio-demographic factors, comorbidities, and treatments like digoxin and oral anticoagulants. This holistic approach allowed for a nuanced understanding of the AF-MCI-dementia trajectory.
The study’s findings are profound. Firstly, it established that AF is associated with a 45% increased risk of developing MCI. This is a significant leap in understanding the cognitive risks associated with AF, a common cardiac arrhythmia. Moreover, the study showed that cardiovascular risk factors and multimorbidity are linked to this increased risk, providing insights into potential intervention points. The implications of these findings are far-reaching. For clinicians, it underscores the importance of vigilant cognitive health monitoring in AF patients. It also suggests that managing cardiovascular risk factors and multimorbidity could be key in preventing or delaying cognitive decline in this population. Furthermore, the study challenges existing paradigms about the relationship between heart health and brain health. It positions AF not just as a cardiac issue but also a potential contributor to cognitive impairment and dementia. This reframing is crucial for developing integrated care approaches that address both cardiac and cognitive health. The significance of the study also lies in its methodological robustness. The large-scale population-based approach, coupled with the detailed analysis of EHR data, lends a high degree of reliability and applicability to the findings. It sets a new standard for epidemiological studies in the field of cognitive health.
In summary, this study is a seminal work in the intersection of cardiology and neurology. It not only elucidates the link between atrial fibrillation and cognitive decline but also prompts a reevaluation of clinical approaches towards AF patients. Management of AF, particularly through anticoagulants to prevent stroke, and controlling other risk factors like hypertension and diabetes, is crucial in potentially reducing the risk of developing dementia. It’s important for patients with AF to work closely with their healthcare providers to manage their condition and reduce their risk of associated complications, including dementia. The study’s revelations about the role of cardiovascular health in cognitive outcomes pave the way for more integrated and proactive strategies in managing patients with atrial fibrillation, with the ultimate goal of preserving cognitive function and quality of life.
Reference
Sheng-Chia Chung, Martin Rossor, Ana Torralbo, Cai Ytsma, Natalie K. Fitzpatrick, Spiros Denaxas, Rui Providencia, Cognitive Impairment and Dementia in Atrial Fibrillation: A Population Study of 4.3 Million Individuals, JACC: Advances, Volume 2, Issue 9, 2023, 100655,
 Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity
Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity

