Significance
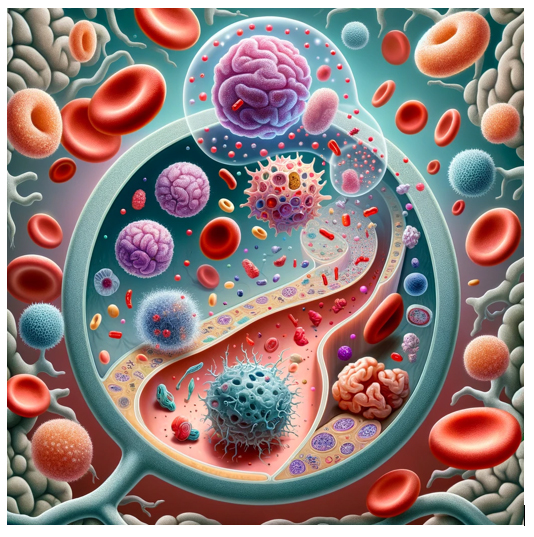
Extracellular vesicles (EVs) are small particles released by cells into the extracellular environment. They are encased in a lipid bilayer and can range in size from 30 to 1000 nanometers. EVs are produced by a variety of cell types and can be found in many bodily fluids, including blood, urine, saliva, and cerebrospinal fluid. These vesicles carry a cargo that includes proteins, lipids, RNA, and DNA, reflecting the physiological state of their cell of origin. EVs play a significant role in cell-to-cell communication and have been implicated in various physiological and pathological processes, including immune responses, angiogenesis, and the spread of cancer. Due to their role in intercellular communication and their presence in easily accessible bodily fluids, EVs have gained significant interest as potential biomarkers for disease diagnosis, prognosis, and therapeutic monitoring. The use of EVs as biomarkers is based on their content, which can change depending on the state of the originating cell. For example, in cancer, tumor-derived EVs can carry specific proteins, DNA mutations, or RNA species that are characteristic of the tumor cells from which they originate. By analyzing the content of EVs isolated from bodily fluids, researchers can potentially identify markers indicative of disease. For clinical applications, methods for isolating and analyzing EVs are being developed and refined. Techniques such as ultracentrifugation, size-exclusion chromatography, and immunoaffinity capture are used to isolate EVs, while tools like flow cytometry, nanoparticle tracking analysis, and various molecular biology techniques are used to analyze their content. Despite the promising potential of EVs as biomarkers, there are challenges to their widespread clinical adoption. These include the need for standardized methods for EV isolation and analysis, as well as further validation of specific EV-based markers for different diseases. As research in this area continues to advance, it is likely that the use of EVs as biomarkers will become more prevalent in clinical diagnostics and personalized medicine. A new study published in Molecular Psychiatry led by Assistant Professor Lena Smirnova, Dr. Sergio Modafferi, Dr. Charlotte Schlett, Dr. Lauren M. Osborne, Dr. Jennifer Payne & Assistant Professor Dr. Sarven Sabunciyan from Johns Hopkins University, the authors addressed a critical gap in psychiatric care: the lack of non-invasive tests for monitoring brain status. Their innovative approach focused on utilizing extracellular vesicles (EVs) and their mRNA contents as potential biomarkers for inferring the state of the brain, particularly in the context of psychiatric disorders.
The researchers developed a bioinformatic approach to identify mRNAs in EVs that are specifically expressed in certain tissues, using tissue-specific gene expression profiles. This method aimed to determine the origin of EV mRNAs found in peripheral blood. The placenta was chosen as a model to validate their approach, where they successfully identified 26 placenta-specific mRNAs in EVs circulating in maternal blood during pregnancy. This confirmed that tissue-specific mRNAs could be detected in blood EVs and used to infer their tissue of origin. Applying the same bioinformatic strategy, the team identified 181 brain-specific mRNAs in EVs from maternal blood, demonstrating the feasibility of detecting brain-derived mRNAs in peripheral blood. A significant finding was the association of 13 brain-specific EV mRNAs with postpartum depression, suggesting the potential of these mRNAs as biomarkers for psychiatric conditions. To further validate their findings, the researchers compared mRNA profiles from cells and EVs within an iPSC-derived brain model, showing a correlation between cellular and extracellular mRNA levels.
The study established the feasibility of using tissue-specific gene expression to identify the origin of EV mRNAs in blood, opening new avenues for biomarker development in psychiatric care. The discovery of 181 brain-specific mRNAs in maternal blood EVs underscores the potential of these mRNAs to reflect brain activity and their implication in psychiatric disorders. The association of specific EV mRNAs with postpartum depression highlights the potential of these biomarkers in diagnosing and monitoring psychiatric conditions. The correlation found between cellular and EV mRNA levels in the brain model suggests the possibility of using peripheral blood EV mRNAs to infer changes in the brain’s transcriptional activity. This research brings to light the potential of EV mRNAs as non-invasive biomarkers for real-time monitoring of psychiatric diseases, facilitating early diagnosis and intervention. The study by Smirnova and her colleagues represents a significant advancement in psychiatric biomarker research. By harnessing the power of EV mRNAs, they have opened a new window into the brain’s state, offering promising prospects for non-invasive, real-time monitoring of psychiatric conditions. This research lays the groundwork for future studies aimed at validating and expanding the use of EV mRNAs as biomarkers in a broader range of psychiatric disorders, moving closer to the goal of precision psychiatry.
Reference
Smirnova L, Modafferi S, Schlett C, Osborne LM, Payne JL, Sabunciyan S. Blood extracellular vesicles carrying brain-specific mRNAs are potential biomarkers for detecting gene expression changes in the female brain. Mol Psychiatry. 2024 Jan 11. doi: 10.1038/s41380-023-02384-6.
 Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity
Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity

