Significance
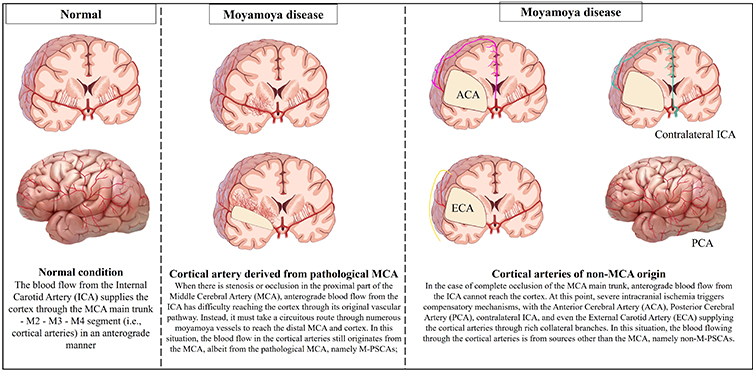
Moyamoya disease (MMD) is a chronic, occlusive cerebrovascular disease characterized by progressive stenosis of the internal carotid arteries and their main branches, leading to the development of a network of abnormal collateral vessels. These vessels, termed “moyamoya” (Japanese for “puff of smoke”), are fragile and can lead to hemorrhagic or ischemic strokes. The disease predominantly affects children and young adults, often leading to severe neurological deficits or death if not properly managed. The assessment of hemodynamic in MMD was primarily focused on the blood flow changes before/after surgery, without detailed investigation into the relationship between the changes and hemodynamic sources of the parasylvian cortical arteries (PSCAs). Understanding the hemodynamic sources of these arteries is crucial, as these are often selected as recipient vessels in extracranial-intracranial (EC-IC) bypass surgeries, a common treatment for MMD. This surgery aims to restore blood flow to the affected areas of the brain, reducing the risk of stroke.
The research team included Dr. Jin Yu, Miao Hu, and led by Professor Jianjian Zhang and Professor Jincao Chen from the Department of Neurosurgery at Zhongnan Hospital of Wuhan University conducted a detailed study to understand the hemodynamic sources of recipient PSCAs in patients with MMD. Their study aimed to assess the relationship of these sources with postoperative cerebral hyperperfusion (CHP) following bypass surgery. The research work is now published in the Frontiers in Neurology Journal. Their study involved a retrospective analysis of adult patients with symptomatic MMD hemispheres admitted between March 2019 and December 2020. The researchers analyzed the hemodynamic sources of the PSCAs using three-dimensional digital subtraction angiography (3D-DSA) combined with magnetic resonance angiography (MRA) fusion imaging. They assessed the spatial and temporal characteristics of the hemodynamic sources of PSCAs and their associations with patients’ demographics, Suzuki stage, and initial onset type.
The authors identified six major types of hemodynamic sources in the PSCAs. This differentiation is significant as it provides insights into the diverse origins of blood supply to these arteries. There was a notable difference in the hemodynamic sources of PSCAs above and below the Sylvian fissure (SF). This finding is crucial because it suggests different patterns of vascular compensation above and below this anatomical landmark. The study found that with advancing Suzuki stages (a grading system used to describe the progression of MMD), there was a notable shift in the blood supply from internal carotid arteries (ICAs) to non-ICAs for PSCAs above the SF. Multivariate analysis indicated that the hemodynamic sources of PSCAs above the SF were significantly associated with patients’ initial onset type (ischemic or hemorrhagic). Understanding these hemodynamic sources can aid in the selection of suitable recipient vessels for bypass surgery, potentially reducing the risk of postoperative CHP.
The findings have several clinical and surgical implications, for example by identifying the types of collateral vessels supplying the PSCAs, surgeons can predict the risk of postoperative CHP, a serious complication that can lead to hemorrhagic strokes post-bypass surgery. Another advantage, the study provided invaluable data for preoperative planning, enabling surgeons to select the most appropriate recipient vessels for bypass surgery, potentially reducing the risk of postoperative complications. The work defined the relationship between the hemodynamic sources of PSCAs and the Suzuki stage of MMD and provided clinicians and researchers better understanding of the progression of the disease and the development of compensatory vascular systems.
This research substantially advances our knowledge of cerebral hemodynamics in MMD. It elucidates the complex patterns of vascular compensation that occur in response to progressive stenosis in intracranial arteries. The study demonstrates a typical conversion trend from internal carotid arteries to non-internal carotid arteries with advancing Suzuki stages, highlighting the dynamic nature of cerebral blood flow in MMD. The global impact of this research is significant, considering the relatively high prevalence of MMD in Asian populations and its increasing recognition worldwide. Future research building on these findings could explore the genetic and molecular mechanisms underlying the development of these collateral pathways, potentially leading to novel therapeutic strategies. In conclusion, the new study by Yu, Hu, Zhang and Chen represents a major step forward in our understanding of MMD. Their innovative approach in analyzing the hemodynamic sources of PSCAs has significant implications for the surgical treatment of MMD, offering a pathway to more personalized and effective interventions.
Reference
Yu J, Hu M, Zhang J, Chen J. Analyzing characteristics of collateral flow to parasylvian cortical arteries by three-dimensional digital subtraction angiography-magnetic resonance angiography fusion imaging in adult moyamoya disease. Front Neurol. 2023;14:1251844. doi: 10.3389/fneur.2023.1251844.
 Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity
Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity



