Significance
In-vitro fertilization (IVF) is the most common technique used in the management of patients with difficulty undergoing conception. The success rate for IVF varies depending on many factors, including the age of the woman, the cause of infertility, and lifestyle factors. The interplay between obesity and reproductive health, particularly in IVF, represents a critical area of research in the field of reproductive medicine. Obesity is now a significant public health concern globally, with its prevalence tripling since 1975 according to the World Health Organization. The impact of obesity extends beyond general health. It can influence various aspects of reproductive outcomes, including fertility, pregnancy, and perinatal outcomes. For instance, adipose tissue can act not only as a fat storage site but also as an active endocrine organ, secreting a range of bioactive molecules, including adipokines, cytokines, and hormones, which can interfere with reproductive processes. Furthermore, obesity is associated with insulin resistance and hyperinsulinemia, conditions that can exacerbate the production of androgens by the ovaries, contributing to conditions such as polycystic ovary syndrome, which can cause of infertility. The insulin resistance characteristic of obesity also impacts the endometrial environment, potentially affecting implantation rates and increasing the risk of miscarriage.
To this account, a new study published in Frontiers in Endocrinology led by Dr. Linda Kluge, Dr. Karin Källén, Dr. Ann Thurin-Kjellberg, Dr. Ulla-Britt Wennerholm, and Dr. Christina Bergh from the Gothenburg University and Sahlgrenska University Hospital in Sweden, the authors, provided a comprehensive examination of the relationship between maternal Body Mass Index (BMI) and various outcomes following IVF. Their objective was to unravel how varying degrees of maternal BMI both the success of IVF in terms of live birth rates and the broader spectrum of maternal and perinatal outcomes. The team carefully constructed a national, population-based cohort study, drawing from an extensive dataset spanning from 2002 to 2020. The study dataset included a large number of IVF cycles, precisely 126,620 fresh cycles and subsequent frozen embryo transfers from 2007 to 2019, alongside 58,187 singleton deliveries from 2002 to 2020. The authors categorized women undergoing IVF based on their BMI, adhering to the World Health Organization’s classifications, ranging from underweight to class III obesity. The study’s robust methodology, including the use of a national, population-based cohort and the adjustment for relevant confounders, lends credibility to its findings.
The authors’ findings painted a vivid picture of the dose-dependent decline in live birth rates with ascending maternal BMI categories. The cumulative live birth rate saw a dip from 32.6% in normal-weight women to 21.1% in women classified under class II and III obesity, signaling a significant impact of maternal weight on IVF success.
The study shed light on the stark increase in maternal and perinatal complications accompanying higher BMI categories. Notably, the risk of hypertensive disorders of pregnancy and preterm births escalated with increasing BMI, underscoring the compounded risks that obesity brings to the table in the context of reproductive outcomes. The research team went the extra mile and conducted as well sensitivity and dropout analyses, to ensure the robustness and reliability of their findings.
According to the authors, the pathophysiological mechanisms underlying these associations are complex and multifactorial. Obesity-related inflammation, altered endometrial receptivity, oxidative stress, and changes in the ovarian follicular environment are among the contributing factors that can impair oocyte quality, fertilization, and embryo development. In conclusion, the new study by Dr. Linda Kluge and her colleagues highlighted the significant impact of maternal BMI on the success of IVF treatments and the subsequent journey of pregnancy and childbirth. The findings echo the critical need for integrated weight management strategies in the preconception care of women undergoing fertility treatments. Weight reduction strategies, including lifestyle modifications, pharmacotherapy, and bariatric surgery, may offer benefits in improving fertility and IVF outcomes.
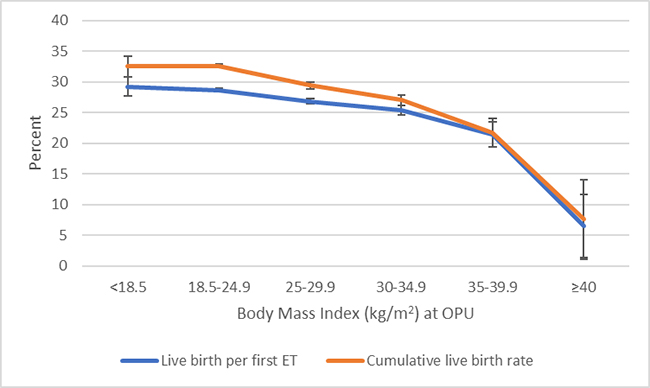
†Cumulative live birth rate: the number of deliveries with at least one live born child
(singleton or multiple) per started fresh IVF cycle, including one fresh and/or all frozen embryo
transfers within one year, until one delivery with a live birth or until all embryos are used, whichever occurred first. BMI = body mass index.
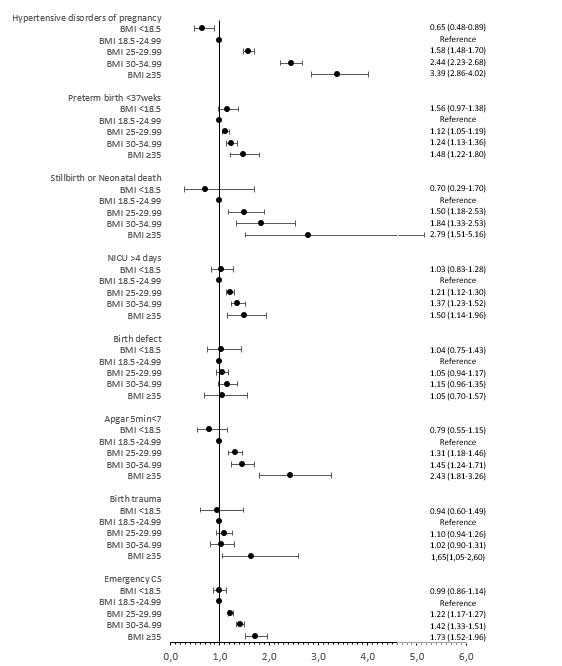
Adjusted for year of treatment (continuous), maternal age (continuous), maternal country of birth
(Sweden/Other European/Outside Europe), maternal educational level (ordinal), fertilisation method (IVF/ICSI)
type of embryo transfer (fresh/frozen), parity (continuous), maternal smoking (yes/no).
BMI = body mass index, CS = caesarean section, NICU = neonatal intensive care unit. (The article was first published in Frontiers in Endocrinology September 11, 2023. )
Reference
Kluge L, Källén K, Thurin-Kjellberg A, Wennerholm UB, Bergh C. The association between body mass index and live birth and maternal and perinatal outcomes after in-vitro fertilization: a national cohort study. Front Endocrinol (Lausanne). 2023;14:1239702. doi: 10.3389/fendo.2023.1239702.
 Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity
Medicine Innovates Medicine Innovates: Delivering innovations in medicine to the world for better health and prosperity

